Description
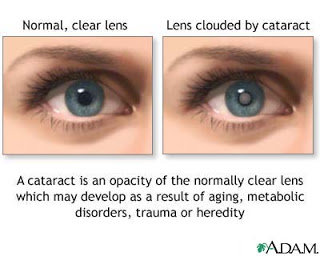
1. A
cataract is an opacity of the lens that distorts image projected onto the
retina and that can progress to blindness.
2. The
lens opacity reduces visual acuity. As the eye ages, the lens loses water and
increases in size and density, causing compression of lens fibers. A cataract
then forms as oxygen uptake is reduced, water content decreases, calcium
content increases, and soluble protein becomes insoluble.
3. Intervention
is indicated when visual acuity has been reduced to a level that the client
finds to be unacceptable or adversely affects lifestyle.
4. Over
time, compression of lens fibers causes a painless, progressive loss of
transparency that is often bilateral. The rate of cataract formation in each
eye is seldom identical.
Causes
§ Cataracts
have several causes and may be age-related, present at birth, or formed as a
result of trauma or exposure to a toxic substance. The most common cataract is
age-related (senile cataract). Traumatic cataracts develop after a foreign body
injures the lens. Complicated cataracts develop as secondary effects in
patients with metabolic disorders (e.g., diabetes mellitus), radiation damage
(x-ray or sunlight), or eye inflammation or disease (e.g., glaucoma, retinitis
pigmentosa, detached retina, recurrent uveitis). Toxic cataracts result from
drug or chemical toxicity. Congenital cataracts are caused by maternal
infection (e.g., German measles, mumps, hepatitis) during the first trimester
of pregnancy.
Complications
§ Complications
may include retinal disorders, pupillary block, adhesions, acute glaucoma,
macular edema, and retinal detachment. Following extracapsular cataract
extraction, the posterior capsule may become opacified. This condition, called
a secondary membrane or after-cataract, occurs when subcapsular lens epithelial
cells regenerate lens fibers, which obstruct vision. After-cataract is treated
by yttrium-aluminum-garnet (YAG) laser treatment to the affected tissue.
Without surgery, a cataract eventually causes complete vision loss.
1. Opaque
or cloudy white pupil
2. Gradual
loss of vision
3. Blurred
vision
4. Decreased
color perception
5. Vision
that is better in dim light with pupil dilation
6. Photophobia
7. Absence
of the red reflex
Primary Nursing Diagnosis
§ Sensory
and perceptual alterations (visual) related to decreased visual acuity
Other Diagnoses that may occur in Nursing Care Plans For
Cataract
§ Anxiety
§ Deficient
knowledge (diagnosis and treatment)
§ Risk
for infection
§ Risk
for injury
Diagnostic Evaluation
§ General
Comments: No specific laboratory tests identify cataracts. Diagnosis is made by
history, visual acuity test, and direct ophthalmoscopic exam.
§ Ophthalmoscopy
or slit lamp examination may reveal a dark area in the red reflex.
Ophthalmoscopy or slit lamp examination is a microscopic instrument that allows
detailed visualization of anterior segment of eye to identify lens opacities
and other eye abnormalities
Medical Management
There is no medical treatment for cataracts, although use of
vitamin C and E and beta-carotene is being investigated. Glasses or contact,
bifocal, or magnifying lenses may improve vision. Mydriatics can be used short
term, but glare is increased.
Surgical Management
§ Surgical
removal of the opacified lens is the only cure for cataracts. The lens can be
removed when the visual deficit is 20/40.
§ If
cataracts occur bilaterally, the more advanced cataract is removed first.
 § Extracapsular
cataract extraction, the most common procedure, removes the anterior lens
capsule and cortex, leaving the posterior capsule intact. A posterior chamber
intraocular lens is implanted where the patient’s own lens used to be.
§ Extracapsular
cataract extraction, the most common procedure, removes the anterior lens
capsule and cortex, leaving the posterior capsule intact. A posterior chamber
intraocular lens is implanted where the patient’s own lens used to be.
§ Intracapsular
cataract extraction removes the entire lens within the intact capsule. An
intraocular lens is implanted in either the anterior or the posterior chamber,
or the visual deficit is corrected with contact lenses or cataract glasses.
§ Complications
may include retinal disorders, pupillary block, adhesions, acute glaucoma,
macular edema, and retinal detachment. Following extracapsular cataract
extraction, the posterior capsule may become opacified. This condition, called
a secondary membrane or after-cataract, occurs when subcapsular lens epithelial
cells regenerate lens fibers, which obstruct vision. After-cataract is treated
by yttrium-aluminum-garnet (YAG) laser treatment to the affected tissue.
Pharmacologic Highlights
§ Acetazolamide
a carbonic anhydrase inhibitor is used to reduce intraocular pressure by
inhibiting times a day inhibitor formation of hydrogen and bicarbonate ions.
§ Phenylephrine
a Sympathomimetic agent causes abnormal dilation of the pupil constriction of
conjunctival arteries.
§ Other
Medications: Postoperatively, medications are prescribed to reduce infection
(gentamicin or neomycin) and to reduce inflammation (dexamethasone), taking the
form of eye drops. Acetaminophen is prescribed for mild discomfort; tropicamide
is prescribed to induce ciliary paralysis.
Nursing Interventions
1. If
nursing care is provided in the patient’s home, structure the environment with
conducive lighting and reduce fall hazards.
2. Suggest
magnifying glasses and large-print books. Explain that sunglasses and soft
lighting can reduce glare.
3. Assist
the patient with the actions of daily living as needed to remedy any self-care
deficit.
4. Encourage
the patient to verbalize or keep a log on his or her fears and anxiety about
visual loss or impending surgery.
5. Help
plan events to solve the problems with social isolation.
Documentation Guidelines
§ Presence
of complications: Eye discharge, pain, vital sign alterations
§ Response
to eye medication
§ Reaction
to supine position
Discharge and Home
Healthcare Guidelines
§ Be sure
the patient understands all medications, including dosage, route, action,
adverse effects, and need for postoperative evaluation, usually the next
day, by the eye surgeon. Review installation technique of eye drops into the
conjunctival sac. Teach the patient to avoid over-the-counter medications,
particularly those with aspirin.
§ Instruct
the patient to report any bleeding, yellow-green drainage, pain, visual losses,
nausea, vomiting, tearing, photophobia, or seeing bright flashes of light.
Instruct the patient to avoid activities that increase intraocular pressure
such as bending at the waist, sleeping on the operativeside, straining with
bowel movements, lifting more than 15 pounds, sneezing, coughing, or vomiting.
Instruct the patient to wear a shield over the operative eye at night to
prevent accidental injury to the eye during sleep and to wear glasses during
the day to prevent accidental injury to the eye while awake. Recommend that the
patient avoid reading for some time after surgery to reduce eye strain and
unnecessary movement so that maximal healing occurs.
§ Advise
the patient not to shampoo for several days after surgery. The face should be
held away from the shower head with the head tilted back so that water spray
and soap avoid contact with the eye.
HOME HEALTH TEACHING
§ Vacuuming
should be avoided because of the forward flexion and rapid, jerky movement
required.
§ Driving,
sports, and machine operation can be resumed when permission is granted by the
eye surgeon.
§ Clients
fitted with cataract eyeglasses need information about altered spatial
perception. The eyeglasses should be first used when the patient is seated,
until the patient adjusts to the distortion.
§ Instruct
the client to look through the center of the corrective lenses and to turn the
head, rather than only the eyes, when looking to the side. Clear vision is
possible only through the center of the lens. Hand-eye coordination movements
must be practiced with assistance and relearned because of the altered spatial
perceptions.
Nursing Care Plan
Nursing Assessment
1. Activity
/ Rest: The change from the usual activities / hobbies in connection with
visual impairment.
2. Neurosensory:
Impaired vision blurred / not clear, bright light causes glare with a gradual
loss of peripheral vision, difficulty focusing work with closely or feel the
dark room. Vision cloudy / blurry, looking halo / rainbow around the beam,
changes eyeglasses, medication does not improve vision, photophobia (acute
glaucoma).
Signs: Looks brownish or milky white in the pupil (cataract), the pupil narrows and red / hard eye and a cloudy cornea (glaucoma emergency, increased tears)
Signs: Looks brownish or milky white in the pupil (cataract), the pupil narrows and red / hard eye and a cloudy cornea (glaucoma emergency, increased tears)
3. Pain /
Leisure: Discomfort light / watery eyes. Sudden pain / heavy persist or
pressure on or around the eyes, headaches.
Nursing Diagnosis
Anxiety related to lack of knowledge.
Goal
1. Lowering
the emotional stress, fear and depression.
2. Acceptance
and understanding instructions surgery.
Nursing Interventions
§ Assess
the degree and duration of visual impairment. Encourage conversation to find
out the patient’s concerns, feelings, and the level of understanding.
§ Rationale:
Information can eliminate the fear of the unknown. Coping mechanisms can help
patients with kegusara compromise, fear, depression, tension, despair, anger,
and rejection.
§ Orient
the patient to the new environment.
§ Rationale:
The introduction to the environment helps reduce anxiety and increase security.
§ Explain
the perioperative routines.
§ Rationale:
Patients who have a lot of information easier to receive treatment and follow
instructions.
§ Describes
intervention much detail as possible.
§ Rationale:
Patients who experience visual disturbances rely on other senses salts input
information.
§ Push to
perform daily living habits when able.
§ Rationale:
Self-care and will increase the sense of healthy independence.
§ Encourage participation of family or the people who matter in
patient care.
§ Rationale:
Patients may not be able to perform all duties in connection with the handling
of personal care.
§ Encourage
participation in social activities and diversion whenever possible (visitors,
radio, audio recording, TV,
crafts, games).
§ Rationale:
Social isolation and leisure time is too long can cause negative feelings.
Nursing Diagnosis
Risk for injury related to blurred vision
Goal
Prevention of injury.
Nursing Interventions
§ Help
the patient when able to do until postoperative ambulation and achieve stable vision and adequate coping
skills, using techniques of vision guidance.
§ Rationale:
Reduce the risk of falling or injury when the step stagger or have no coping
skills for vision impairment.
§ Help
the patient set the environment.
§ Rationale:
Providing facilities of independence and lower the risk of injury.
§ Orient
the patient in the room.
§ Rationale:
Improving safety and mobility in the environment.
§ Discuss
the need for the use of metal shields or goggles when instructed
§ Rationale:
shield or goggles protect the eyes against injury.
§ Do not
put pressure on the affected eye trauma.
§ Rationale:
The pressure in the eye may cause further serious damage.
§ Use
proper procedures when providing eye drugs.
§ Rationale:
Injury can occur if the container touch the eye medication.
Nursing Diagnosis
Acute pain related to trauma to the incision and increased IOP
Goal
Reduction of pain and the IOP.
Nursing Interventions
§ Give
medications to control pain and the IOP as prescribed.
§ Rationale:
Use the recipe will
reduce pain and the IOP and increase comfort.
§ Give cold compress on demand for blunt trauma.
§ Rationale:
reduce the edema will reduce the pain.
§ Reduce
the level of lighting
§ Rationale:
The level of lighting is more lower after surgery.
§ Encourage
use of sunglasses in strong light.
§ Rationale:
Strong light causes discomfort after use of eye drops dilator.
Nursing Diagnosis
Risk for infection related to trauma to the incision
Goal
Complications can be avoided or promptly reported to the doctor.
Nursing Interventions
§ Maintain
strict aseptic technique, do
wash your hands frequently.
§ Rationale:
It would minimize infection.
§ Supervise
and report immediately any signs
and symptoms of complications, such as: bleeding, increased IOP or
infection.
§ Rationale:
The discovery of early complications can reduce the risk of permanent vision
loss.
§ Explain
the recommended position.
§ Rationale:
Elevation of the head and avoid lying on the side of the operation may reduce
the edema.
§ Instruct
the patient to know bedrest activity restrictions, with flexibility to the
bathroom, according to a gradual increase in activity tolerance.
§ Rationale:
Limitation of activity prescribed to speed healing and avoid further damage to
the injured eye.
§ Describe
the actions that should be avoided, as prescribed by coughing, sneezing,
vomiting (ask for medication for it).
§ Rationale:
It can lead to complications such as vitreous prolapse or dehiscence injury due
to increased tension on the suture wounds that are very subtle.
§ Give
medications as prescribed, according to prescribed techniques.
§ Rationale:
Drugs are administered in a way that is inconsistent with prescriptions can
interfere with healing or cause complications.













0 comments:
Post a Comment