Description
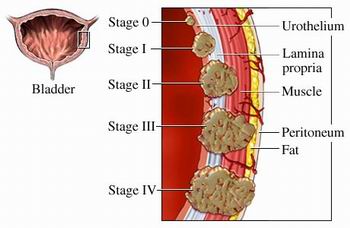
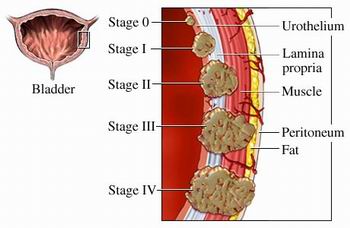
- Bladder cancer is papillomatous growth in the bladder urothelium that undergo malignant changes and that may infiltrate the bladder wall.
- Predisposing factors include cigarette smoking, exposure to industrial chemicals and exposure to radiation.
- Common signs of metastasis include the liver, bones and lungs
- As the tumor progresses can extend to the rectum, vagina and retro- peritoneal structures.
Assessment
- Painless hematuria
- Dysuria
- Gross hematuria
- Obstruction of urine flow
- Development of fistula ( urine from the vagina, fecal material in the urine)
Diagnostic Evaluation
Biopsies of the tumor and adjacent mucosa are definitive, but the following procedures are also used:
- Cystoscopy, biopsy of tumor and adjacent mucosa
- Excretory urography
- Computed CT Scan
- Ultrasonography
- Bimanual examination by anesthesia
- Cytologic evaluation of fresh urine and saline bladder washings
Molecular assays, bladder tumor antigens, adhesion molecules and others are being studied.
Primary Nursing Diagnosis
- Risk for altered urinary elimination related to the obstruction of urinary flow
Medical Management
Radiation
- Most bladder cancer are poorly radio sensitive and require high doses of radiation
- Radiation therapy is more acceptable for advance disease that cannot be eradicated by surgery.
- Palliative radiation maybe used to relieve pain and bowel obstruction and control potential hemorrhage and leg edema cause by venous or lymphatic obstruction.
- Intracavitary radiation maybe prescribed which protect adjacent tissues.
- External radiation combined with chemotherapy or surgery maybe prescribed because the external radiation alone maybe ineffective.
- Complications of radiations:
- A bacterial cystitis
- Proctitis
- Fistula formation
- Ileitis or colitis
- Bladder ulceration and hemorrhage
Chemotherapy
1. Intravesical instillation
- An alkylating chemotherapeutic agent is instilled into the bladder
- This method provides an concentrated topical treatment with little systemic absorption
- Chemotherapeutic agents used may include thiotepa, mitomycin (Mutamycin), doxorubicin (Adriamycin), cyclophosphamide (Cytoxan), and bacille Calmette-Guerin.
- The medication is injected into a urethral catheter and retain for two hours.
- Following instillation, the clients position is rotated every 15 to 30 minutes, starting in the supine position to avoid lying on full bladder.
- After 2 hours, the client voids in a sitting position and is instructed to increase fluids to flash the bladder.
- Treat the urine as biohazard and send to radioisotope laboratory for monitoring.
- For 6 hours following intravesical therapy, disinfect the toilet with household bleach after the client has voided.
2. Systemic chemotherapy
- Systemic chemotherapy is used to treat inoperable or late tumors.
- Agents used may include, cysplatin (Platinol), doxorubicin (Adremycin), cyclophospamide (Cytosan), methotrexate (Folex) and Pyridoxine
3. Complications of chemotherapy
- Bladder irritation
- Hemorrhagic cystitis
Surgical Interventions
1. Transurethral resection of the bladder
- Local resection and fulguration ( destruction of tissue by electrical current through electrodes place in direct contact with the tissue)
- Perform for early tumor for cure or for inoperable tumors for palliation.
2. Partial Cystectomy
- Partial cystectomy is the removal of up to half of the bladder
- The procedure is done for early tumors and for clients who cannot tolerate radical cystectomy.
- During the initial postoperative period bladder capacity is reduced greatly to about 60 mL; however, as the bladder tissue expand, the capacity increases to 200 -400 mL.
- Maintenance of a continuous output of urine following surgery is critical to prevent bladder distention and stress on the suture line.
- A urethral catheter and a suprapubic catheter maybe in place, in the suprapubic catheter maybe left in place for 2 weeks until healing occurs.
3. Cystectomy and urinary diversion
- The procedure involves removal of the bladder and urethra in the women, and the bladder, the urethra, and usually the prostrate and seminal vesicles in men.
- When the bladder and urethra are remove, permanent urinary diversion is required.
- The surgery meybe performed into stages if the tumor is expensive, with the creation of the urinary diversion first and the cystectomy several weeks later.
- If a radical cystectomy is performed lower extremity lymphedema may occur as a result of lymp node dissection, and impotence may occur in the may client.
4. Ileal conduit
- The ileal conduit also is called ureteroileostomy or Bricker’s procedure.
- Ureters are implanted into a segment of the ileum, with the formation of an abdominal stoma.
- The urine flows into the conduit and is propelled continually out through the stoma by peristalsis.
- The client is required to wear an appliance over the stoma to collect the urine.
- Complications include obstruction, pyelonephritis, leakage at the anastomosis site, stenosis, hydronephrosis, calculuses, skin irritation and ulceration, and stomal defects.
5. Kock pouch
- The Koch pouch is a continent internal ileal reservoir created from a segment of the ileum and ascendingcolon.
- The ureters are implanted into the side of the reservoir, and a special nipple valve is constructed to attach the reservoir to the skin.
- Postoperatively, the client will have a 24 to 26 Foley catheter in place to drain urine continuously until the pouch has healed.
- The catheter is irrigated gently with NS to prevent obstruction from mucus or clots.
- Following removal of the catheter, the client is instructed in how to self-catheterize and to drain the reservoir at 4 to 6 hour intervals.
6. Indiana pouch
- A continent reservoir is created from the ascending colon and terminal ileum, making a pouch larger than the Koch pouch.
- Postoperatively, the client will have a 24 to 26 Foley catheter inplace to drain urine continuously until the pouch has healed.
- The Foley catheter is irrigated gently with NS to prevent obstruction from mucus or clots.
- Following removal of the Foley catheter, the client is instructed in how to self-catheterize and to drain the reservoir at 4 to 6 hour intervals.
7. Creation of a neobladder
- Creation of a neobladder is similar to the creation of an internal reservoir, with the difference being that instead of emptying through an abdominal stoma, the bladder empties through a pelvic outlet into the urethra.
- The client empties the neobladder by relaxing the external sphincter and creating abdominal pressure or by intermittent self- catheterization.
8. Percutaneous nephrostomy or pyelostomy
- These procedures are used when the cancer is inoperable to prevent obstruction.
- The procedures involve a percutaneous or surgical insertion of a nephrostomy tube into the kidney for drainage.
- Nursing interventions involves stabilizing the tube to prevent dislodgement and monitoring output.
9. Ureterostomy
- Ureterostomy may be performed as a palliative procedure if the ureters are obstructed by the tumor.
- The ureters are attached to the surface of the abdomen, where the urine flows directly into a drainage appliance without a conduit.
- Potential problems include infection, skin irritation,and obstruction to urinary flow as a result of strictures at the opening.
10. Vesicostomy
- The bladder is sutured to the abdomen, and a stoma is created in the bladder wall.
- The bladder empties through the stoma.
Pharmacologic Intervention
- Chemotheraphy with a combination of methotrexate, 5-fluorouracil (5-FU), vinblastine, doxorubicin (Adriamycin), and cisplatin (M-VAC) and new agents gemcitabine and taxane, possibly by topical chemotheraphy applied directly to the bladder wall
- Intravesical BCG (effective with superficial transitional cell carcinoma)
- Cytotoxic agent infusions through the arterial supply of the involved organ
- Formalin, phenol, or silver nitrate instillations to achieve relief of hematuria and strangury (slow and painful discharge of urine) in some patients
Nursing Intervention
For patients who require radical cystectomy with urinary diversion, offer support and reinforcement of the information. Be sure what to expect. Involve another family member in the preoperative education. If it is needed, arrange a preoperative visit by someone who has adjusted well to a similar diversion.
If any type of stoma is to be created, arrange for a preoperative visit from the enterostomal therapist. The enterostomal therapist can assist in the selection and marking of the stoma site (although the stoma site is somewhat contingent upon the type of urinary diversion to be performed) and can introduce the patient to the external urine collection pouch and related care.
Preoperative interventions
- Administer bowel preparation as prescribed, which may include a clear liquid diet, laxatives and enemas, and antibiotics to lower the bacterial count in the bowel.
- Assist the surgeon and the enterostomal nurse in selecting an appropriate skin site for creation of the abdominal stoma.
- Encourage the client to talk about his or her feelings related to the stoma creation.
Postoperative interventions
- Monitor Vital signs.
- Assess incision site.
- Assess stoma (should be red and moist) every hour for the first 24 hours.
- Monitor for edema in the stoma, which may be present in the immediate postoperative period.
- If the stoma appears dark and dusky, notify the physician immediately because this indicates necrosis
- Monitor for prolapse or retraction of the stoma.
- Assess for return of bowel function; monitor for peristalsis, which will return in 3 to 4 days.
- Maintain NPO status as prescribed until bowel sounds return.
- Monitor urine flow, which is continuous (30 to 60 mL per hour) following surgery.
- Notify the physician if the urine output is less than 30 mL an hour or if no urine output occurs for more than 15 minutes.
- Ureteral stents or catheters may be in place for 2 to 3 weeks or until healing occurs; maintain stability with catheters to prevent dislodgment.
- Monitor urinary output closely and irrigate catheter (if present ) gently to prevent obstruction, as prescribed, with 60 mL of NS.
- Monitor for hematuria.
- Monitor for signs of peritonitis.
- Monitor for bladder distention following a partial cystectomy.
- Monitor for shock, hemorrhage, thrombophlebitis, and lower extremity lymphedema following a radical cystectomy.
- Monitor the urinary drainage pouch for leaks, and check skin integrity.
- Monitor the pH of the urine (do not place the dipstick in the stoma) because strong alkali urine can cause skin irritation and facilitate crystal formation.
- Instruct the client regarding the potential for urinary tract infection or the development of the calculuses.
- Instruct the client to assess the skin for irritation and to monitor the urinary drainage pouch for any leakage.
- Encourage the client to express feelings about changes in body image, embarrassment, and sexual dysfunction.
Documentation Guidelines
- Description of all dressings, wounds, and drainage-collection devices
- Physical findings related to the pulmonary assessment, abdominal assessment, presence of edema, condition of extremities, bowel and bladder patterns of voiding
- Response to and side effects experienced related to intravesical instillations of chemotherapy or BCG; systemic chemotherapy
- Teaching performed, the patient’s understanding of the content, the patient’s ability to perform procedures demonstrated
Discharge and Home Healthcare Guidelines
PATIENT TEACHING
- Following creation of an ileal conduit, teach the patient and significant others the care of the stoma and urinary drainage system. If needed, arrange for follow-up home nursing care or visits with an enterostomal therapist.
- Teach the patient the specific procedure to catheterize the continent cutaneous pouch or reservoir. A simple stoma covering made from a feminine hygiene pad can be worn between catheterizations.
- Stress the need for the patient to wear a medical ID bracelet.
- Following orthotopic bladder replacement, teach the patient how to irrigate the Foley catheter. Suggest the use of a leg bag during the day and a Foley drainage bag at night. Once the pouch has healed and the Foley catheter, ureteral stents, and pelvic drain have been removed, teach the patient to “push” or “bear down” with each voiding.
- Instruct the patient on methods for performing Kegel exercises during and between voidings to minimize incontinence. Suggest wearing incontinence pads until full control is achieved.
- Also instruct the patient on self-catheterization techniques in case the patient is unable to void. Instruct patients where to obtain ostomy pouches, catheters, and other supplies. Teach the patient how to clean and store catheters between use following the clean technique.
CARE OF SKIN IN EXTERNAL RADIATION FIELD
- Encourage the patient to verbalize concerns about radiation therapy, and reassure the patient that she or he is not “radioactive.” Instruct the patient to wash skin gently with mild soap, rinse with warm water, and pat the skin dry each day but not to wash off the ink marking that outlines the radiation field.
- Encourage the patient to avoid applying any lotions, perfumes, deodorants, or powder to the treatment area.
- Encourage the patient to wear nonrestrictive soft cotton clothing directly over the treatment area and to protect the skin from sunlight and extreme cold.
- Stress the need to maintain the schedule for follow-up visits and disease surveillance as recommended by the physician.
Nursing Care Plan
Nursing Diagnosis:
Risk for infection related to inadequate defenses, secondary and immune system (the effect of chemotherapy / radiation), malnutrition, invasive procedures.
Goals:
- Patients are able to identify and participate in infection prevention measures.
- Showed no signs of infection and wound healing normally takes place.
Nursing Interventions :
- Wash hands before taking action. Visitors are also encouraged to do the same.
- Maintain a good personal hygine
- Monitor the temperature
- Examine all the systems to look for signs of infection
- Avoid / limit invasive procedures and maintain aseptic procedures
- Collaborative
- Give antibiotics when indicated.
Nursing Diagnosis
Risk for Sexual Dysfunction related to deficit of knowledge / skills about alternative responses to health transition, decreased function / structure, the effects of treatment.
Goals:
- Patients may express its understanding of the effects of cancer and treatment on sexuality.
- Maintaining sexual activity within your limits
Nursing Interventions:
- Discuss with patients and families about sexuality and the reactionprocess and its relationship with disease
- Give advise on the effect of treatment on sexuality
- Give privacy to the patient and her partner. Knock before entering.
Nursing Diagnosis:
Risk for Impaired Skin Integrity related to the effects of radiation and chemotherapy, immunologic deficits, decreased nutrient intake and anemia.
Goals:
- Patients can identify interventions related to specific conditions
- Participate in the prevention of complications and accelerated healing
Nursing Interventions:
- Assess the integrity of the skin to see any side effects of cancer therapy, wound healing observed.
- Instruct patient not to scratch the itch
- Change the position of the patient on a regular basis
- Give advise patients to avoid the use of skin creams, oils, powders without medical advice
 Definition
Definition 