Description
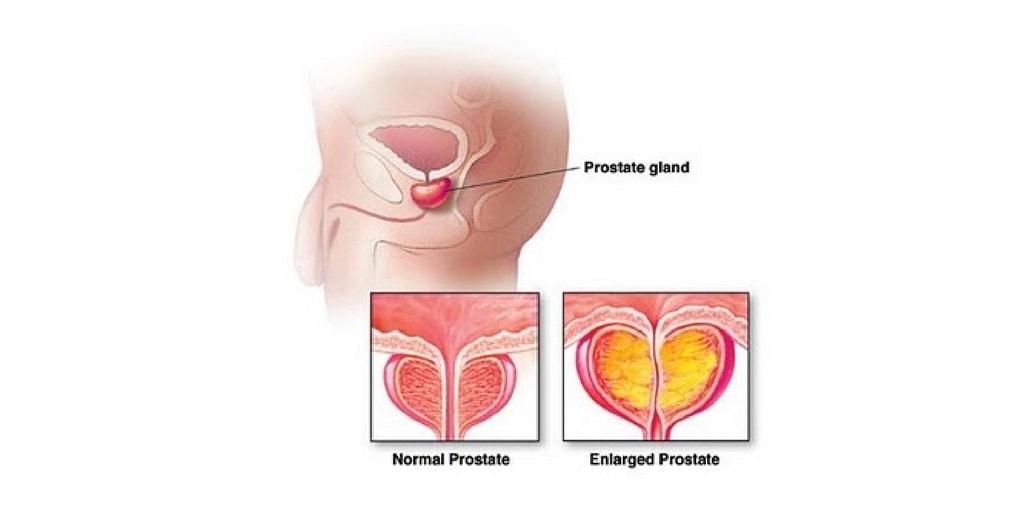
- A slow enlargement of the prostate gland occurs, with hypertrophy and hyperplasia of normal tissue.
- The enlargement causes narrowing of the urethra and results in partial or complete obstruction.
- The cause is unknown, and the disorder usually occurs in men older than 50 years.
Causes
Because the condition occurs in older men, changes in hormone balances have been associated with the cause. Androgens (testosterone) and estrogen appear to contribute to the hyperplastic changes that occur. Other theories, such as those involving diet, heredity, race, and history of chronic inflammation, have been associated with BPH, but no definitive links have been made with these potential contributing factors.
Assessment
- Urgency, frequency, and hesitancy
- Changes in sizes and force of urinary stream
- Retention
- Dribbling
- Nocturia
- Hematuria
- Urinary stasis
- UTIs
Physical Examination
Inspect and palpate the bladder for distension. A digital rectal exam (DRE) reveals a rubbery enlargement of the prostate, but the degree of enlargement does not consistently correlate with the degree of urinary obstruction. Some men have enlarged prostates that extend out into soft tissue without compressing the urethra. Determine the amount of pain and discomfort that is associated with the DRE.
The International Prostate Symptom Score
- Incomplete emptying: Over the past month, how often have you had the sensation of not emptying your bladder completely after you have finished urinating? (Not at all _ 0, less than 1 time in 5 _ 1, less than half the time _ 2, about half the time _ 3, more than half the time _ 4, almost always _ 5)
- Frequency: Over the past month, how often have you had to urinate again less than 2 hours after you finished urinating? (Not at all _ 0, less than 1 time in 5 _ 1, less than half the time _ 2, about half the time _ 3, more than half the time _ 4, almost always _ 5)
- Intermittency: Over the past month, how often have you stopped and started again several times when urinating? (Not at all _ 0, less than 1 time in 5 _ 1, less than half the time _ 2, about half the time _ 3, more than half the time _ 4, almost always _ 5)
- Urgency: Over the past month, how often have you found it difficult to postpone urination? (Not at all _ 0, less than 1 time in 5 _ 1, less than half the time _ 2, about half the time _ 3, more than half the time _ 4, almost always _ 5)
Diagnostic Evaluation
- Physical examination, including digital rectal examination (DRE).
- Urinalysis and urodynamic studies to determine obstructed flow
- Renal function tests, including serum creatinine levels
- Complete blood studies, including clotting studies
Primary Nursing Diagnosis
- Urinary retention (acute or chronic) related to bladder obstruction
Medical Management
The treatment plan depends in the cause, severity of obstruction, and condition of the patient. Treatment measures include:
- Immediate catheterization if patient cannot void (a urologist may be consulted if an ordinary catheter cannot be inserted). A suprapubic cystostomy is sometimes necessary.
- “Watchful waiting” to monitor disease progression.
- Balloon dilation or alpha-1 adrenergic receptor blockers (terazosin) to relax smooth muscle of the bladder neck and prostate
- Hormonal manipulation with antiandrogen (finasteride [Proscar]) decreases the size of the prostate and improves urinary flow.
- Saw palmetto is a botanical remedy for mild to moderate BPH.
Surgical Management
- Transurethral laser resection with ultrasound guidance
- Transurethral needle ablation (spares urethra, nerves, muscles, and membranes)
- Microwave thermotheraphy (using transurethral probe) applied to hypertrophied tissue, which then becomes necrotic and sloughs off
Surgical procedures such as prostatectomy can be used to remove the hypertrophied portion of the prostrate gland. Other kinds of surgery include:
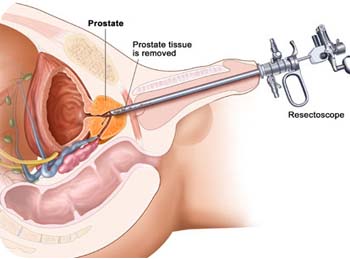
- Transurethral resection of the prostrate (TUR or TURP); urethral endoscopic procedure is most common approach.
- Suprapubic prostatectomy (perineal incision); incontinence, impotence, or rectal injury may be complications
- Retropubic prostatectomy (low abdominal incision)
Pharmacologic Intervention
- Phenoxybenzamine (alpha-adrenergic) 10 mg PO bid, to blocks effects of postganglionic blocker synapses at the smooth muscle and exocrine glands; improvement of urinary flow in 75% of patients
- Finasteride (5-alpha reductase) 5 mg PO qd, to shrinks prostate gland and improves inhibitor urine flow
- Other Medications: Prazosin, alfuzosin, doxazosin
Nursing Intervention
- Encourage fluid intake of up to 2000 to 3000 mL per day unless contraindicated.
- Prepare for bladder drainage via urinary catheterization for distention.
- Avoid administering medications that case urinary retention, such as anticholinergics, antihistamines, and decongentants.
- Administer finasteride (proscar) as prescribes to shrink the prostate gland and improve urine flow.
- Prepare the client for surgery as prescribed.
Surgical interventions for Benign Prostatic Hyperplasia
- Perineal prostatectomy
- Retropubic prostatectomy
- Suprapubic prostatectomy
- Transurethral resection of the prostate
Postoperative Care Following Transurethral Resection of the Prostate
Continuous Bladder Irrigation (CBI)
- A three- way (lumen) irrigation is used to decrease bleeding and to keep the bladder free from clots:
- One lumen for inflating the balloon (30mL)
- One lumen for installation (inflow)
- One lumen for outflow
Interventions
- Maintain traction on the catheter if applied to prevent bleeding by pulling the catheter taut and tapping it to the abdomen or thigh.
- Instruct the client to keep the leg straight if traction is applied to the catheter and it is taped to the thigh.
- Catheter traction is not release without a physician’s order and usually is released after any bright red drainage has diminished.
- Use normal saline or prescribed solution only to prevent water intoxication.
- Run the solution at a rate, as prescribed, to keep the urine pink.
- Run the solution rapidly if bright red drainage or clots are present.
- Run the solution at about 40 gtt/min when the bright red drainage clears.
- If the urinary catheter becomes obstructed, turn off the CBI and irrigate the catheter wit 30 to 50 mL of normal saline if prescribed; notify physician if obstruction does not resolve.
- Monitor for transurethral resection syndrome or severe hyponatremia (water intoxication) caused by the excessive absorption of bladder irrigation during surgery (altered mental status, bradycardia , increase blood pressure, and confusion).
- Discontinue CBI and Foley catheter as prescribed, usually 24 to 48 hours after surgery.
- Monitor for continence and urinary retention when the catheter is removed.
- Inform the client that some burning, frequency, and dribbling may occur following catheter removal.
- Inform the client that he should be voiding 150 to 200 mL of clear yellow urine every 3 to 4 hours by 3 days after surgery.
- Inform the client that he may pass small clots and tissue debris for several days.
- Teach the client to avoid heavy lifting, stressful exercise, driving, Valsalva’s maneuver, and sexual intercourse for 2 to 6 weeks to prevent strain, and to call the physician if bleeding occurs or there is a decreased in urinary stream.
- Instruct the client to drink 2400 to 3000 mL of fluid each day, preferably before 8PM
- Instruct the client to avoid alcohol, caffeinated beverages, and spicy foods and avoid overstimulation of the bladder
- Instruct the client that if the urine becomes bloody, to rest and increase fluid intake, and that if the bleeding does not subside, to notify the physician.
Documentation Guidelines
- Presence of urinary discomfort, bleeding, frequency, retention, or difficulty initiating flow
- Presence of bladder distension, discomfort, and incontinence
- Intake and output; color of urine, presence of clots, quality of urine (clear versus cloudy)
- Presence of complications: Urinary retention, bleeding, infection
- Reaction to information regarding sexual function
Discharge and Home Healthcare Guidelines
- PATIENT TEACHING. Instruct patients about the need to maintain a high fluid intake (at least 2 L/day) to ensure adequate urine output. Teach the patient to monitor urinary output for 4 to 6 weeks after surgery to ensure adequacy in volume of elimination combined with a decrease in volume of retention.
- MEDICATIONS. Provide instructions about all medications used to relax the smooth muscles of the bladder or to shrink the prostate gland. Provide instructions on the correct dosage, route, action, side effects, and potential drug interactions and when to notify these to the physician.
- PREVENTION. Instruct the patient to report any difficulties with urination to the physician immediately. Explain that BPH can recur and that he should notify the physician if symptoms of urgency, frequency, difficulty initiating stream, retention, nocturia, or bladder distension recur.
- POSTOPERATIVE. Encourage the patient to discuss any sexual concerns he or his partner may have after surgery with the appropriate counselors. Reassure the patient that a session can be set up by the nurse or physician whenever one is indicated. Usually, the physician recommends that the patient have no sexual intercourse or masturbation for several weeks after invasive procedures.
Nursing Care Plan
Nursing Diagnosis: Urinary Retention
May be related to:
- Mechanical obstruction; enlarged prostate
- Decompensation of detrusor musculature
- Inability of bladder to contract adequately
Possibly evidenced by:
- Frequency, hesitancy, inability to empty bladder completely; incontinence/dribbling
- Bladder distension, residual urine
Desired Outcomes
- Void in sufficient amounts with no palpable bladder distension.
- Demonstrate postvoid residuals of less than 50 mL, with absence of dribbling/overflow.
Nursing Interventions
Independent
- Encourage patient to void every 2–4 hr and when urge is noted.
- Rationale: May minimize urinary retention/overdistension of the bladder.
- Ask patient about stress incontinence when moving, sneezing, coughing, laughing, lifting objects.
- Rationale: High urethral pressure inhibits bladder emptying or can inhibit voiding until abdominal pressure increases enough for urine to be involuntarily lost.
- Observe urinary stream, noting size and force.
- Rationale: Useful in evaluating degree of obstruction and choice of intervention.
- Have patient document time and amount of each voiding. Note diminished urinary output. Measure specific gravity as indicated
- Rationale: Urinary retention increases pressure within the ureters and kidneys, which may cause renal insufficiency. Any deficit in blood flow to the kidney impairs its ability to filter and concentrate substances.
- Percuss and palpate suprapubic area.
- Rationale: A distended bladder can be felt in the suprapubic area.
- Encourage oral fluids up to 3000 mL daily, within cardiac tolerance, if indicated.
- Rationale: Increased circulating fluid maintains renal perfusion and flushes kidneys, bladder, and ureters of “sediment and bacteria.” Note: Initially, fluids may be restricted to prevent bladder distension until adequate urinary flow is reestablished.
- Monitor vital signs closely. Observe for hypertension, peripheral/dependent edema, changes in mentation. Weigh daily. Maintain accurate I&O.
- Rationale: Loss of kidney function results in decreased fluid elimination and accumulation of toxic wastes; may progress to complete renal shutdown.
- Provide/encourage meticulous catheter and perineal care.
- Rationale: Reduces risk of ascending infection.
- Recommend sitz bath as indicated.
- Rationale: Promotes muscle relaxation, decreases edema, and may enhance voiding effort.
Collaborative
- Administer medications as indicated: androgen inhibitors, e.g., finasteride (Proscar);
- Rationale: Reduces the size of the prostate and decreases symptoms if taken long-term; however, side effects such as decreased libido and ejaculatory dysfunction may influence patient’s choice for long-term use.
- Alpha-adrenergic antagonists, e.g., tamsulosin (Flomax), prazosin (Minipress), terazosin (Hytrin), doxazosin mesylate (Cardura)
- Rationale: Studies indicate that these drugs may be as effective as Proscar for outflow obstruction and may have fewer side effects in regard to sexual function.
- Antispasmodics, e.g., oxybutynin (Ditropan)
- Rationale: Relieves bladder spasms related to irritation by the catheter.
- Rectal suppositories (B & O)
- Rationale: Suppositories are absorbed easily through mucosa into bladder tissue to produce muscle relaxation/relieve spasms.
- Antibiotics and antibacterials.
- Rationale: Given to combat infection. May be used prophylactically.
- Catheterize for residual urine and leave indwelling catheter as indicated.
- Rationale: Relieves/prevents urinary retention and rules out presence of ureteral stricture. Coudé catheter may be required because the curved tip eases passage of the tube through the prostatic urethra. Note: Bladder decompression should be done with caution to observe for sign of adverse reaction, e.g., hematuria (rupture of blood vessels in the mucosa of the overdistended bladder) and syncope (excessive autonomic stimulation).
- Irrigate catheter as indicated.
- Rationale: Maintains patency/urinary flow.
Monitor laboratory studies:
- BUN, Cr, electrolytes
- Rationale : Prostatic enlargement (obstruction) eventually causes dilation of upper urinary tract (ureters and kidneys), potentially impairing kidney function and leading to uremia.
- Urinalysis and culture
- Rationale : Urinary stasis potentiates bacterial growth, increasing risk of UTI.
- Prepare for/assist with urinary drainage, e.g., cystostomy.
- Rationale: May be indicated to drain bladder during acute episode with azotemia or when surgery is contraindicated because of patient’s health status.
Prepare for surgical intervention
- Balloon urethroplasty/transurethral dilation of the prostatic urethra
- Rationale: Inflation of a balloon-tipped catheter within the obstructed area stretches the urethra and displaces prostatic tissue, thus improving urinary flow.
- Transurethral incision of the prostate (TUIP).
- Rationale: A procedure of almost equivalent efficacy to transurethral resection of the prostate (TURP) used for prostates with estimated resected tissue weight of 30 g or less. It may be performed instead of balloon dilation with better outcomes. Procedure can be done in ambulatory or short-stay settings. Note: Open prostate resection procedures (TURP) are typically performed on patients with very large prostate glands.
- Transurethral microwave thermotherapy (TUMT).
- Rationale: Heating the central portion of the prostate by the insertion of a heating element through the urethra destroys prostate cells. Treatment is usually completed in a one-time procedure carried out in the physician’s office.
Nursing Diagnosis: Acute pain
May be related to:
- Mucosal irritation: bladder distension, renal colic
- Urinary infection
- Radiation therapy
Possibly evidenced by:
- Reports of pain (bladder/rectal spasm)
- Narrowed focus; altered muscle tone, grimacing; distraction behaviors, restlessness
- Autonomic responses
Desired Outcomes
- Report pain relieved/controlled.
- Appear relaxed.
- Be able to sleep/rest appropriately.
Nursing Interventions
Independent
- Assess pain, noting location, intensity (scale of 0–10), duration.
- Rationale: Provides information to aid in determining choice/effectiveness of interventions.
- Tape drainage tube to thigh and catheter to the abdomen (if traction not required).
- Rationale: Prevents pull on the bladder and erosion of the penile-scrotal junction.
- Recommend bedrest as indicated.
- Rationale: Bedrest may be needed initially during acute retention phase; however, early ambulation can help restore normal voiding patterns and relieve colicky pain.
- Provide comfort measures, e.g., back rub, helping patient assume position of comfort. Suggest use of relaxation/deep-breathing exercises, diversional activities.
- Rationale: Promotes relaxation, refocuses attention, and may enhance coping abilities.
- Encourage use of sitz baths, warm soaks to perineum.
- Rationale: Promotes muscle relaxation.
Collaborative
- Insert catheter and attach to straight drainage as indicated.
- Rationale: Draining bladder reduces bladder tension and irritability.
- Instruct in prostatic massage.
- Rationale: Aids in evacuation of ducts of gland to relieve congestion/inflammation. Contraindicated if infection is present.
- Administer medications as indicated:Narcotics, e.g., meperidine (Demerol)
- Rationale: Given to relieve severe pain, provide physical and mental relaxation.
- Antibacterials, e.g., methenamine hippurate (Hiprex)
- Rationale: Reduces bacteria present in urinary tract and those introduced by drainage system.
- Antispasmodics and bladder sedatives, e.g., flavoxate (Urispas), oxybutynin (Ditropan).
- Rationale: Relieves bladder irritability.
Nursing Diagnosis: Risk for Fluid Volume Deficiency
May be related to:
- Postobstructive diuresis from rapid drainage of a chronically overdistended bladder
- Endocrine, electrolyte imbalances (renal dysfunction)
Possibly evidenced by:
- presence of signs and symptoms establishes an actual diagnosis
Desired Outcomes
- Maintain adequate hydration as evidenced by stable vital signs, palpable peripheral pulses, good capillary refill, and moist mucous membranes.
Nursing Interventions
Independent
- Monitor output carefully. Note outputs of 100–200 mL/hr.
- Rationale: Rapid/sustained diuresis could cause patient’s total fluid volume to become depleted and limits sodium reabsorption in renal tubules.
- Encourage increased oral intake based on individual needs.
- Rationale: Patient may have restricted oral intake in an attempt to control urinary symptoms, reducing homeostatic reserves and increasing risk of dehydration/hypovolemia.
- Monitor BP, pulse. Evaluate capillary refill and oral mucous membranes.
- Rationale: Enables early detection of and intervention for systemic hypovolemia.
- Promote bedrest with head elevated.
- Rationale: Decreases cardiac workload, facilitating circulatory homeostasis.
Collaborative
- Monitor electrolyte levels, especially sodium.
- Rationale: As fluid is pulled from extracellular spaces, sodium may follow the shift, causing hyponatremia.
- Administer IV fluids (hypertonic saline) as needed.
- Rationale: Replaces fluid and sodium losses to prevent/correct hypovolemia following outpatient procedures.
Nursing Diagnosis: Fear/ Anxiety
May be related to:
- Change in health status: possibility of surgical procedure/malignancy
- Embarrassment/loss of dignity associated with genital exposure before, during, and after treatment; concern about sexual ability.
Possibly evidenced by:
- Increased tension, apprehension, worry
- Expressed concerns regarding perceived changes
- Fear of unspecific consequences
Desired Outcomes
- Appear relaxed.
- Verbalize accurate knowledge of the situation.
- Demonstrate appropriate range of feelings and lessened fear.
- Report anxiety is reduced to a manageable level.
Nursing Interventions
Independent
- Be available to patient. Establish trusting relationship with patient/SO.
- Rationale: Demonstrates concern and willingness to help. Encourages discussion of sensitive subjects.
- Provide information about specific procedures and tests and what to expect afterward, e.g., catheter, bloody urine, bladder irritation. Be aware of how much information patient wants
- Rationale: Helps patient understand purpose of what is being done, and reduces concerns associated with the unknown, including fear of cancer. However, overload of information is not helpful and may increase anxiety.
- Maintain matter-of-fact attitude in doing procedures/dealing with patient. Protect patient’s privacy.
- Rationale: Communicates acceptance and eases patient’s embarrassment.
- Encourage patient/SO to verbalize concerns and feelings.
- Rationale: Defines the problem, providing opportunity to answer questions, clarify misconceptions, and problem-solve solutions.
- Reinforce previous information patient has been given.
- Rationale: Allows patient to deal with reality and strengthens trust in caregivers and information presented
Nursing Diagnosis: Knowledge, deficient [Learning Need] regarding condition, prognosis, treatment, self-care, and discharge needs.
May be related to:
- Lack of exposure/recall, information misinterpretation
- Unfamiliarity with information resources
- Concern about sensitive area
Possibly evidenced by:
- Questions, request for information; verbalization of the problem
- Inappropriate behaviors, e.g., apathetic, withdrawn
- Inaccurate follow-through of instructions, development of preventable complications
Desired Outcomes
- Knowledge: Disease Process
- Verbalize understanding of disease process/prognosis and potential complications.
- Identify relationship of signs/symptoms to the disease process.
- Knowledge: Treatment Regimen
- Verbalize understanding of therapeutic needs.
- Initiate necessary lifestyle/behavior changes.
- Participate in treatment regimen.
Nursing Interventions
Independent: (Teaching: Disease Process)
- Review disease process, patient expectations.
- Rationale: Provides knowledge base from which patient can make informed therapy choices.
- Encourage verbalization of fears/feelings and concerns.
- Rationale: Helping patient work through feelings can be vital to rehabilitation.
- Give information that the condition is not sexually transmitted.
- Rationale: May be an unspoken fear.
- Review drug therapy/use of herbal products and diet, e.g., increased fruits, soy beans.
- Rationale: Some patients may prefer to treat with complementary therapy because of decreased occurrence/lessened severity of side effects, e.g. impotence.
- Recommend avoiding spicy foods, coffee, alcohol, long automobile rides, rapid intake of fluids (particularly alcohol).
- Rationale:May cause prostatic irritation with resulting congestion. Sudden increase in urinary flow can cause bladder distension and loss of bladder tone, resulting in episodes of acute urinary retention.
- Address sexual concerns, e.g., during acute episodes of prostatitis, intercourse is avoided, but may be helpful in treatment of chronic condition.
- Rationale: Sexual activity can increase pain during acute episodes but may serve as massaging agent in presence of chronic disease. Note: Medications such as finasteride (Proscar) are known to interfere with libido and erections. Alternatives include terazosin (Hytrin), doxazosin mesylate (Cardura), and tamsulosin (Flomax), which do not affect testosterone levels.
- Provide information about basic sexual anatomy. Encourage questions and promote a dialogue about concerns.
- Rationale: Having information about anatomy involved helps patient understand the implications of proposed treatments because they might affect sexual performance.
- Review signs/symptoms requiring medical evaluation, e.g., cloudy, odorous urine; diminished urinary output, inability to void; presence of fever/chills.
- Rationale: Prompt interventions may prevent more serious complications.
- Discuss necessity of notifying other healthcare providers of diagnosis.
- Rationale: Reduces risk of inappropriate therapy, e.g., use of decongestants, anticholinergics, and antidepressants, which can increase urinary retention and may precipitate an acute episode.
- Reinforce importance of medical follow-up for at least 6 mo to 1 yr, including rectal examination, urinalysis.
- Rationale: Recurrence of hypertrophy and/or infection (caused by same or different organisms) is not uncommon and requires changes in therapeutic regimen to prevent serious complications.











0 comments:
Post a Comment