Description
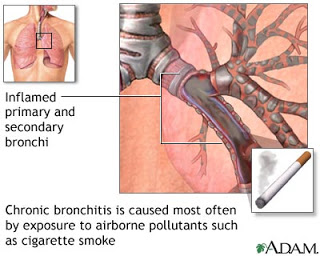
- Is an inflammation of the lower airways characterized by excessive secretion of mucus, hypertrophy of mucous glands, and recurring infection, progressing to narrowing and obstruction of airflow.
Causes/ Risk Factors
- The primary cause of chronic bronchitis is smoking or exposure to some type of respiratory irritant. Established risk factors include a history of smoking, occupational exposures, air pollution,reduced lung function, and heredity. Children of parents who smoke are at higher risk for pulmonary infections that may lead to bronchitis.
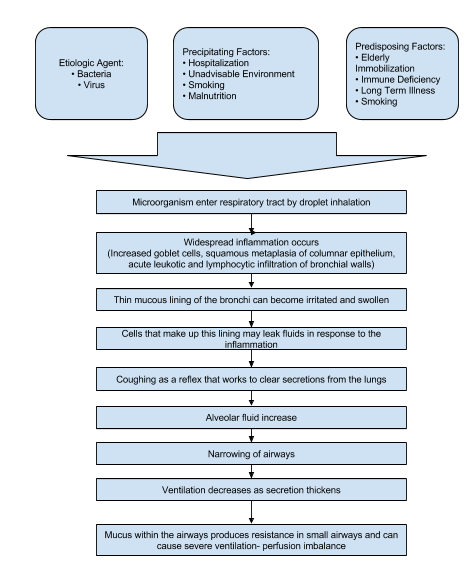
Pathophysiology
Assessment
- Signs and symptoms of chronic bronchitis (insidious onset):
- Productive cough lasting at least 3 months during a year for 2 successive years.
- Thick, gelatinous sputum (greater amounts produced during superimposed infections).
- Dyspnea and wheezing as disease progresses.
Diagnostic Evaluation
- Pulmonary function tests, to demonstrate airflow obstruction-reduced forced expiratory volume in 1 second (FEV1), FEV1 to forced vital capacity ratio; increased residual volume to total lung capacity (TLC) ration, possibly increased TLC.
- Chest X-rays to detect hyperinflation, flattened diaphragm, increased retrosternal space, decreased vascular markings, possible bullae (all in late stages).
- Arterial blood gases, to detect decreased arterial oxygen pressure (PaO2), pH, and increased arterial carbon dioxide pressure (Paco2).
- Sputum smears and cultures to identify pathogens.
Primary Nursing Diagnosis
- Impaired gas exchange related to obstructed airways
Therapeutic Intervention / Medical Management
- Smoking cessation to stop the progression and preserve lung capacity.
- Low-flow oxygen to correct severe hypoxemia in a controlled manner and minimize carbon dioxide retention.
- Home oxygen therapy, especially at night to prevent turnal oxygen desaturation.
- Pulmonary rehabilitation to reduce symptoms that limit activity.
- Chest physical therapy, including postural drainage and breathing retraining.
- Lung transplant in severe cases of alpha1-antitrypsin deficiency.
Pharmacologic Intervention
- Bronchodilators to reduce dyspnea and control bronchospasm delivered by metered-dose inhaler, other handheld devices, or nebulization.
- Inhaled corticosteriods may be useful for some with severe airflow limitation and frequent exacerbations.
- Corticosteroids by mouth or I.V. in acute exacerbations.
- Antimicrobials to control secondary bacterial infections in the bronchial tree, thus clearing the airways.
- Alpha1-antitrypsin replacement delivered by I.V. infusion.
Nursing Intervention
- Monitor for adverse effects of bronchodilators-tremulousness, tachycardia, cardiac arrhythmias, central nervous system stimulation, hypertension.
- Monitor oxygen saturation at rest and with activity.
- Eliminate all pulmonary irritants, particularly cigarette smoke. Smoking cessation usually reduces pulmonary irritation, sputum production, and cough. Keep the patient’s room as dust-free as possible.
- Use postural drainage positions to help clear secretions responsible for airway obstruction.
- Teach controlled coughing.
- Encourage high level of fluid intake (8 to 10 glasses; 2 to 2.5 L daily) within level of cardiac reserve.
- Give inhalations of nebulized saline to humidify bronchial tree and liquefy sputum. Add moisture (humidifier, vaporizer) to indoor air.
- Avoid dairy products if these increase sputum production.
- Encourage the patient to assume comfortable position to decrease dyspnea.
- Use pursed lip breathing at intervals and during periods of dyspnea to control rate and depth of respiration and improve respiratory muscle coordination.
- Discuss and demonstrates relaxation exercises to reduce stress, tension, and anxiety.
- Encourage frequent small meals if the patient is dyspneic; en a small increase in abdominal contents may press on diaphragm and impede breathing.
- Offer liquid nutritional supplements to improve caloric intake and counteract weight loss.
- Avoid foods producing abdominal discomfort.
- Encourage use of portable oxygen system for ambulation for patients with hypoxemia and marked disability.
- Encourage the patient in energy conservation techniques.
Documentation Guidelines
- Respiratory status of the patient: Respiratory rate, breath sounds, use of oxygen, color of nail beds and lips; note any respiratory distress
- Response to activity: Degree of shortness of breath with any exertion,degree of fatigue
- Comfort, body temperature
- Response to medications, oxygen,and breathing treatments
- Need for assistance with activities of daily living
- Response to diet and increased caloric intake, daily weights
Discharge and Home Healthcare Guidelines
- Medications. Be sure that the patient understands all medications, including the dosage, route, action, and adverse effects. Patients on aminophylline should have blood levels drawn as ordered by the physician. Before being discharged from the hospital, the patient should demon- strate the proper use of metered-dose inhalers.
- Complications. Instruct patients to notify their primary healthcare provider of any change in the color or consistency of their secretions. Green-colored secretions may indicate the pres- ence of a respiratory infection. Patients should also report consistent, prolonged periods of dyspnea that are unrelieved by medications.
- Follow-up. Consider that patients with severe disease may need assistance with activities of daily living after discharge. Note any referrals to social services. Send patients home with a diet, provided by the dietitian and reinforced by the nurse, which provides a high-caloric intake. Encourage the patient to cover the face with a scarf if he or she goes out-of-doors in the winter. If the patient continues to smoke,provide the name of a smoking cessation program or a support group. Encourage the patient to avoid irritants in the air.
Nursing Care Plan
Ineffective Airway Clearance
Assessment
Patient may manifest
- Wheezes/crackles on auscultation on the BLF
- Subcostal retraction
- Nasal flaring
- Presence of non-productive cough
- Increase RR above normal range
Nursing Diagnosis
- Ineffective Airway Clearance
Outcomes
- Patient will demonstrate effective clearing of secretions.
- Patient will maintain effective airway clearance.
Nursing Interventions
- Position head midline with flexion on appropriate for age/condition
- Rationale: To gain or maintain open airway
- Elevate HOB
- Rationale: To decrease pressure on the diaphragm and enhancing drainage
- Observe S/Sx of infections
- Rationale: To identify infectious process
- Auscultate breath sounds & assess air mov’t
- Rationale: To ascertain status & note progress
- Instruct the patient to increase fluid intake
- Rationale: To help to liquefy secretions.
- Demonstrate effective coughing and deep-breathing techniques.
- Rationale: To maximize effort
- Keep back dry
- Rationale: To prevent further complications
- Turn the patient q 2 hours
- Rationale: To prevent possible aspirations
- Demonstrate chest physiotherapy, such as bronchial tapping when in cough, proper postural drainage.
- Rationale: These techniques will prevent possible aspirations and prevent any untoward complications
- Administer bronchodilators if prescribed.
- Rationale: More aggressive measures to maintain airway patency.
Ineffective Breathing Pattern
Assessment
Patient may manifest
- Wheezes/crackles on auscultation on the BLF
- Subcostal retraction
- Nasal flaring
- Presence of non-productive cough
- Increase RR above normal range
Nursing Diagnosis
- Ineffective Breathing Pattern RT Retained Secretions
Outcomes
- Patient will improve breathing pattern.
- Patient will maintain a respiratory rate within normal limits.
Nursing Interventions
- Place patient in semi-fowlers position
- Rationale: To have a maximum lung expansion
- Increase fluid intake as applicable
- Rationale: To liquefy secretions
- Keep patient back dry
- Rationale: To avoid stasis of secretions and avoid further complication
- Change position every 2 hours
- Rationale: To facilitate secretion mov’t and drainage
- Perform CPT
- Rationale: To loosen secretion
- Place a pillow when the client is sleeping
- Rationale: To provide adequate lung expansion while sleeping.
- Instruct how to splint the chest wall with a pillow for comfort during coughing and elevation of head over body as appropriate
- Rationale: To promote physiological ease of maximal inspiration
- Maintain a patent airway, suctioning of secretions may be done as ordered
- Rationale: To remove secretions that obstructs the airway
- Provide respiratory support. Oxygen inhalation is provided per doctor’s order
- Rationale: To aid in relieving patient from dyspnea
- Administer prescribed cough suppressants and analgesics and be cautious, however, because opioids may depress respirations more than desired.
- Rationale: To promote deeper respirations and cough
Impaired Gas Exchange
Assessment
Patient may manifest
- Appearance of bluish extremities when in cough (cyanosis), lips
- Lethargy
- Restlessness
- Hypercapnea
- Hypoxemia
- Abnormal rate, rhythm, depth of breathing
- Diaphoresis
Nursing Diagnosis
- Impaired Gas Exchange RT Altered Oxygen Balance
Outcomes
- Patient will improve ventilation and adequate oxygenation of tissues
- Patient will minimize or totally be free of symptoms of respiratory distress.
Nursing Interventions
- Monitor level of consciousness or mental status
- Rationale: Restlessness,anxiety, confusion, somnolence are common manifestation of hypoxia and hypoxemia.
- Assist the client into the High-Fowlers position
- Rationale: The upright position allows full lung excursion and enhances air exchange
- Increase patient’s fluid intake
- Rationale: To help liquefy secretions
- Encourage expectoration
- Rationale: To eliminate thick, tenacious, copious secretions which contribute for the impairment of gas exchange.
- Encourage frequent position changes
- Rationale: To promote drainage of secretions
- Encourage adequate rest & limit activities to within client tolerance
- Rationale: Helps limit oxygen needs/consumption
- Promote calm/restful environments
- Rationale: To correct/improve existing deficiencies
- Administer supplemental oxygen judiciously as indicated
- Rationale: May correct or prevent worsening of hypoxia.
- Administer meds as indicated such as bronchodilators
- Rationale: To treat the underlying condition
Sleep Pattern Disturbance
Assessment
Patient may manifest
- Irritability
- Restlessness
- Lethargy
- Changes in posture
- Difficulty of breathing which worsens at night
Nursing Diagnosis
- Sleep Pattern Disturbance RT Difficulty of Breathing
Outcomes
- Patient will identify individually appropriate interventions to promote sleep.
- Patient will be able to report improvements in sleep/rest pattern.
Nursing Interventions
- Monitor level of consciousness or mental status
- Rationale: Restlessness, anxiety,confusion, somnolence are common manifestation of hypoxia and hypoxemia.
- Promote comfort measures such as back rub and change in position as necessary
- Rationale: To provide non pharmacologic management
- Observe provision of emotional support
- Rationale: Lack of knowledge and problems, relationships may create tension. Interfering with sleep routines based on adult schedules may not meet child’s needs.
- Provide quiet environment.
- Rationale: To promote an environment conducive to sleep.
- Increase patient’s fluid intake
- Rationale: To help liquefy secretions
- Encourage expectoration
- Rationale: To eliminate thick, tenacious, copious secretions which contribute for the DOB
- Limit the fluid intake in evening if nocturia is a problem
- Rationale: To reduce need for nighttime elimination
- Obtain feedback from SO regarding usual bedtime, rituals/routines
- Rationale: To determine usual sleep patterns & provide comparative baseline
- Provide safety for patient sleep time safety
- Rationale: To promote comfort/safety
- Recommend mid morning nap if one required
- Rationale: Napping esp. in the afternoon can disrupt normal sleep pattern
- Administer pain medication as ordered.
- Rationale: To relieve discomfort and take maximum advantage of sedative effect
Risk for Spread of Infection
Assessment
Patient may manifest
- Body temperature above normal range
- Dehydration
- Increase WBC count
- Presence of increase mucus production
Nursing Diagnosis
- Risk for Spread of Infection RT Stasis of Secretions & Decreased Ciliary Action
Outcomes
- Patient will identify interventions to prevent and/or reduce the risk of infection
- Patient will have minimize or totally be free from the risk of infection.
Nursing Interventions
- Review importance of breathing exercises, effective cough, frequent position changes, and adequate fluid intake
- Rationale: These activities promote mobilization and expectoration of secretions to reduce the risk of developing pulmonary infection.
- Turn the patient q 2 hours
- Rationale: To facilitate secretion mov’t and drainage
- Encourage increase fluid intake
- Rationale: To liquefy secretions
- Stress the importance of handwashing to SO’s
- Rationale: Handwashing is the primary defense against the spread of infection
- Teach the SO’s how to care for and clean respiratory equipment
- Rationale: Water in respiratory equipment is a common source of bacterial growth
- Teach the SO’s the manifestations of pulmonary infections (change in color of sputum, fever, chills) , self-care and when to call the physician
- Rationale: Early recognition of manifestations can lead to a rapid diagnosis.
- Recommend rinsing mouth with water
- Rationale: To prevent risk of oral candidiasis.
- Administer antimicrobial such as cefuroxime as indicated.
- Rationale: Given prophylactically to reduce any possible complications
Other Possible Nursing Care Plans
- High risk for suffocation
- High risk for aspiration
- Anxiety RT acute breathing difficulties
- Activity Intolerance RT inadequate oxygenation
- Imbalanced Nutrition: Less than body requirements RT reduced appetite and dyspnea (for emphysema)











0 comments:
Post a Comment