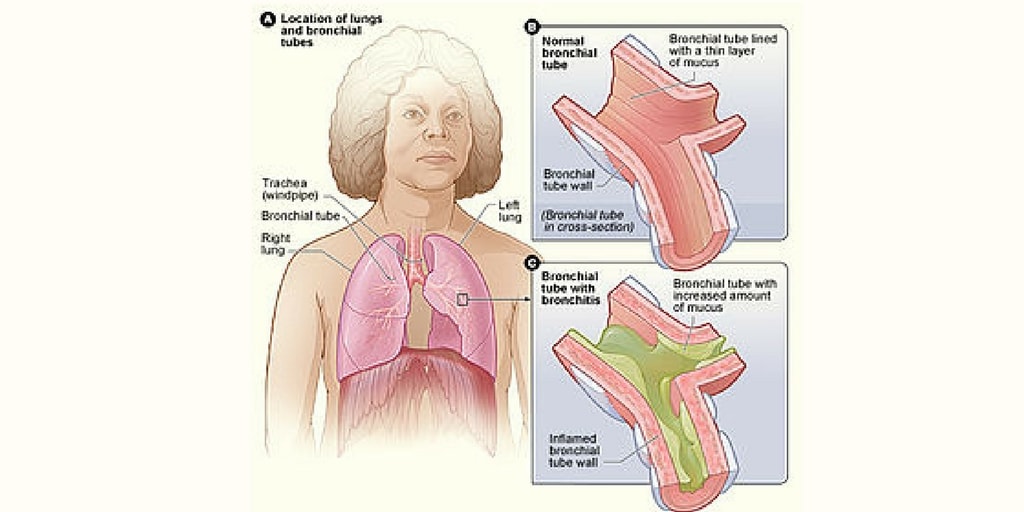
Description
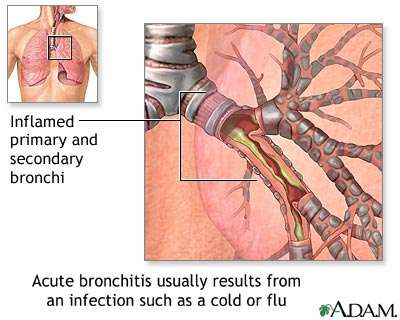
- Is an infection of the lower respiratory tract that generally follows an upper respiratory tract infection. As a result of this viral (most common) or bacterial infection, the airways become inflamed and irritated, and mucus production increases.
Causes
- Acute bronchitis is usually caused by viruses. Established risk factors include a history of smoking, occupational exposures, air pollution, reduced lung function, and heredity. Children of parents who smoke are at higher risk for pulmonary infections that may lead to bronchitis.
Assessment:
- Fever, tachypnea, mild dyspnea, pleuritic chest pain (possible).
- Cough with clear to purulent sputum production.
- Diffuse rhonchi and crackles(contrast with localized crackles usually heard with pneumonia).
Diagnostic Evaluation:
- Chest X-ray may rule out pneumonia. In bronchitis, films show no evidence of lung infiltrates or consolidation.
Primary Nursing Diagnosis
- Impaired gas exchange related to obstructed airways
Medical Management:
- Chest physiotherapy to mobilize secretions, if indicated.
- Hydration to liquefy secretions.
Pharmacologic Interventions:
- Inhaled bronchodilators to reduce bronchospasm and promote sputum expectoration.
- A course of oral antibiotics such as a macrolide may be instituted, but is controversial.
- Symptom management for fever and cough.
Nursing Interventions:
- Encourage mobilization of secretion through ambulation, coughing, and deep breathing.
- Ensure adequate fluid intake to liquefy secretions and prevent dehydration caused by fever and tachypnea.
- Encourage rest, avoidance of bronchial irritant, and a good diet to facilitate recovery.
- Instruct the patient to complete the full course of prescribed antibiotics and explain the effect of meals on drug absorption.
- Caution the patient on using over-the-counter cough suppressants, antihistamines, and decongestants, which may cause drying and retention of secretions. However, cough preparations containing the mucolytic guaifenesin may be appropriate.
- Advise the patient that a dry cough may persist after bronchitis because of irritation of airways. Suggest avoiding dry environments and using a humidifier at bedside. Encourage smoking cessation.
- Teach the patient to recognize and immediately report early signs and symptoms of acute bronchitis.
Documentation Guidelines
- Respiratory status of the patient: Respiratory rate, breath sounds, use of oxygen, color of nail beds and lips; note any respiratory distress
- Response to activity: Degree of shortness of breath with any exertion,degree of fatigue
- Comfort, body temperature
- Response to medications, oxygen,and breathing treatments
- Need for assistance with activities of daily living
- Response to diet and increased caloric intake, daily weights
Discharge and Home Healthcare Guidelines
- Medications. Be sure that the patient understands all medications, including the dosage, route, action, and adverse effects. Patients on aminophylline should have blood levels drawn as ordered by the physician. Before being discharged from the hospital, the patient should demon- strate the proper use of metered-dose inhalers.
- Complications. Instruct patients to notify their primary healthcare provider of any change in the color or consistency of their secretions. Green-colored secretions may indicate the pres- ence of a respiratory infection. Patients should also report consistent, prolonged periods of dyspnea that are unrelieved by medications.
- Follow-up. Consider that patients with severe disease may need assistance with activities of daily living after discharge. Note any referrals to social services. Send patients home with a diet, provided by the dietitian and reinforced by the nurse, which provides a high-caloric intake. Encourage the patient to cover the face with a scarf if he or she goes out-of-doors in the winter. If the patient continues to smoke,provide the name of a smoking cessation program or a support group. Encourage the patient to avoid irritants in the air.
Nursing Care Plan
Ineffective Airway Clearance
Assessment
Patient may manifest
- Wheezes/crackles on auscultation on the BLF
- Subcostal retraction
- Nasal flaring
- Presence of non-productive cough
- Increase RR above normal range
Nursing Diagnosis
- Ineffective Airway Clearance
Outcomes
- Patient will demonstrate effective clearing of secretions.
- Patient will maintain effective airway clearance.
Nursing Interventions
- Position head midline with flexion on appropriate for age/condition
- Rationale: To gain or maintain open airway
- Elevate HOB
- Rationale: To decrease pressure on the diaphragm and enhancing drainage
- Observe S/Sx of infections
- Rationale: To identify infectious process
- Auscultate breath sounds & assess air mov’t
- Rationale: To ascertain status & note progress
- Instruct the patient to increase fluid intake
- Rationale: To help to liquefy secretions.
- Demonstrate effective coughing and deep-breathing techniques.
- Rationale: To maximize effort
- Keep back dry
- Rationale: To prevent further complications
- Turn the patient q 2 hours
- Rationale: To prevent possible aspirations
- Demonstrate chest physiotherapy, such as bronchial tapping when in cough, proper postural drainage.
- Rationale: These techniques will prevent possible aspirations and prevent any untoward complications
- Administer bronchodilators if prescribed.
- Rationale: More aggressive measures to maintain airway patency.
Ineffective Breathing Pattern
Assessment
Patient may manifest
- Wheezes/crackles on auscultation on the BLF
- Subcostal retraction
- Nasal flaring
- Presence of non-productive cough
- Increase RR above normal range
Nursing Diagnosis
- Ineffective Breathing Pattern RT Retained Secretions
Outcomes
- Patient will improve breathing pattern.
- Patient will maintain a respiratory rate within normal limits.
Nursing Interventions
- Place patient in semi-fowlers position
- Rationale: To have a maximum lung expansion
- Increase fluid intake as applicable
- Rationale: To liquefy secretions
- Keep patient back dry
- Rationale: To avoid stasis of secretions and avoid further complication
- Change position every 2 hours
- Rationale: To facilitate secretion mov’t and drainage
- Perform CPT
- Rationale: To loosen secretion
- Place a pillow when the client is sleeping
- Rationale: To provide adequate lung expansion while sleeping.
- Instruct how to splint the chest wall with a pillow for comfort during coughing and elevation of head over body as appropriate
- Rationale: To promote physiological ease of maximal inspiration
- Maintain a patent airway, suctioning of secretions may be done as ordered
- Rationale: To remove secretions that obstructs the airway
- Provide respiratory support. Oxygen inhalation is provided per doctor’s order
- Rationale: To aid in relieving patient from dyspnea
- Administer prescribed cough suppressants and analgesics and be cautious, however, because opioids may depress respirations more than desired.
- Rationale: To promote deeper respirations and cough
Impaired Gas Exchange
Assessment
Patient may manifest
- Appearance of bluish extremities when in cough (cyanosis), lips
- Lethargy
- Restlessness
- Hypercapnea
- Hypoxemia
- Abnormal rate, rhythm, depth of breathing
- Diaphoresis
Nursing Diagnosis
- Impaired Gas Exchange RT Altered Oxygen Balance
Outcomes
- Patient will improve ventilation and adequate oxygenation of tissues
- Patient will minimize or totally be free of symptoms of respiratory distress.
Nursing Interventions
- Monitor level of consciousness or mental status
- Rationale: Restlessness,anxiety, confusion, somnolence are common manifestation of hypoxia and hypoxemia.
- Assist the client into the High-Fowlers position
- Rationale: The upright position allows full lung excursion and enhances air exchange
- Increase patient’s fluid intake
- Rationale: To help liquefy secretions
- Encourage expectoration
- Rationale: To eliminate thick, tenacious, copious secretions which contribute for the impairment of gas exchange.
- Encourage frequent position changes
- Rationale: To promote drainage of secretions
- Encourage adequate rest & limit activities to within client tolerance
- Rationale: Helps limit oxygen needs/consumption
- Promote calm/restful environments
- Rationale: To correct/improve existing deficiencies
- Administer supplemental oxygen judiciously as indicated
- Rationale: May correct or prevent worsening of hypoxia.
- Administer meds as indicated such as bronchodilators
- Rationale: To treat the underlying condition
Sleep Pattern Disturbance
Assessment
Patient may manifest
- Irritability
- Restlessness
- Lethargy
- Changes in posture
- Difficulty of breathing which worsens at night
Nursing Diagnosis
- Sleep Pattern Disturbance RT Difficulty of Breathing
Outcomes
- Patient will identify individually appropriate interventions to promote sleep.
- Patient will be able to report improvements in sleep/rest pattern.
Nursing Interventions
- Monitor level of consciousness or mental status
- Rationale: Restlessness, anxiety,confusion, somnolence are common manifestation of hypoxia and hypoxemia.
- Promote comfort measures such as back rub and change in position as necessary
- Rationale: To provide non pharmacologic management
- Observe provision of emotional support
- Rationale: Lack of knowledge and problems, relationships may create tension. Interfering with sleep routines based on adult schedules may not meet child’s needs.
- Provide quiet environment.
- Rationale: To promote an environment conducive to sleep.
- Increase patient’s fluid intake
- Rationale: To help liquefy secretions
- Encourage expectoration
- Rationale: To eliminate thick, tenacious, copious secretions which contribute for the DOB
- Limit the fluid intake in evening if nocturia is a problem
- Rationale: To reduce need for nighttime elimination
- Obtain feedback from SO regarding usual bedtime, rituals/routines
- Rationale: To determine usual sleep patterns & provide comparative baseline
- Provide safety for patient sleep time safety
- Rationale: To promote comfort/safety
- Recommend mid morning nap if one required
- Rationale: Napping esp. in the afternoon can disrupt normal sleep pattern
- Administer pain medication as ordered.
- Rationale: To relieve discomfort and take maximum advantage of sedative effect
Risk for Spread of Infection
Assessment
Patient may manifest
- Body temperature above normal range
- Dehydration
- Increase WBC count
- Presence of increase mucus production
Nursing Diagnosis
- Risk for Spread of Infection RT Stasis of Secretions & Decreased Ciliary Action
Outcomes
- Patient will identify interventions to prevent and/or reduce the risk of infection
- Patient will have minimize or totally be free from the risk of infection.
Nursing Interventions
- Review importance of breathing exercises, effective cough, frequent position changes, and adequate fluid intake
- Rationale: These activities promote mobilization and expectoration of secretions to reduce the risk of developing pulmonary infection.
- Turn the patient q 2 hours
- Rationale: To facilitate secretion mov’t and drainage
- Encourage increase fluid intake
- Rationale: To liquefy secretions
- Stress the importance of handwashing to SO’s
- Rationale: Handwashing is the primary defense against the spread of infection
- Teach the SO’s how to care for and clean respiratory equipment
- Rationale: Water in respiratory equipment is a common source of bacterial growth
- Teach the SO’s the manifestations of pulmonary infections (change in color of sputum, fever, chills) , self-care and when to call the physician
- Rationale: Early recognition of manifestations can lead to a rapid diagnosis.
- Recommend rinsing mouth with water
- Rationale: To prevent risk of oral candidiasis.
- Administer antimicrobial such as cefuroxime as indicated.
- Rationale: Given prophylactically to reduce any possible complications
Other Possible Nursing Care Plans
- High risk for suffocation
- High risk for aspiration
- Anxiety RT acute breathing difficulties
- Activity Intolerance RT inadequate oxygenation
- Imbalanced Nutrition: Less than body requirements RT reduced appetite and dyspnea (for emphysema)











0 comments:
Post a Comment